- The outer proportion of the meniscus contains mainly type 1 collagen compared to the inner portion that contains 60% type II and 40% type I
- Therefore the outer proportion of the meniscus is more fibrous and withstands tensile stress but has low compressive and torsional stiffness. The inner portion is able to withstand compression better.
- The menisci are microscopically arranged into three distinct layers: superficial, lamellar and deep.
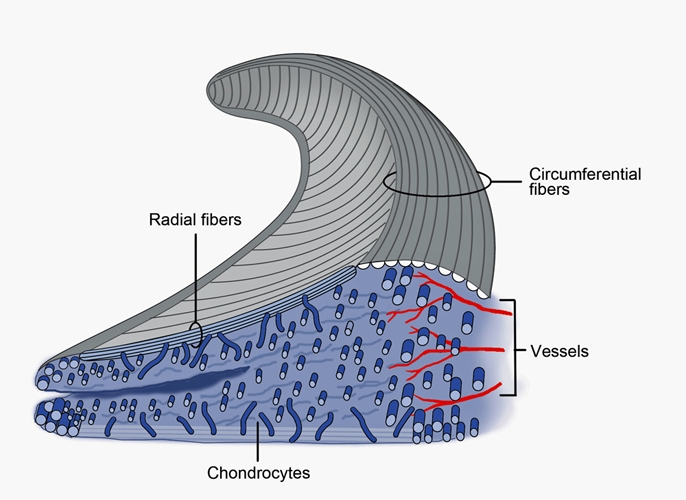
Figure 2. A cross-section of the meniscus showing the radial and circumferential collagen fiber orientation. Numerous bundles of circumferentially oriented Type I collagen fibers are dispersed throughout the meniscus giving its highest tensile strength in that direction. Other collagen fibers are oriented radially and woven into the circumferential bundles. There are also some superficial fibers with random orientation creating a mesh-like matrix on the femoral articular surface.
- The superficial layer exists on both the tibial and femoral surfaces. It is composed of an unorganised random arrangement of collagen fibrils in the superior region and more radially orientated fibres in the inferior region. This surface arrangement allows the meniscus to slide optimally along the articulating surfaces of both the femoral condyles and tibial plateau.
- Underneath the reticular is a lamellar layer that also exists on both the femoral and tibial sides. These fibres are variable in direction with a predominantly radial orientation at the periphery and at the anterior and posterior horns. Despite the presence of radial fibres, random fibre orientation dominates the lamellar zone.
- The main part of the meniscal tissue is located between the two lamellar layers. A dense framework of circumferential coarse type I collagen fibreslies in this layer, cross-linked with radial fibres from the periphery. The radial fibres may act as a “tie” holding the circumferential fibres together, providing structural rigidity against compressive forces and resisting longitudinal splitting of the menisci.
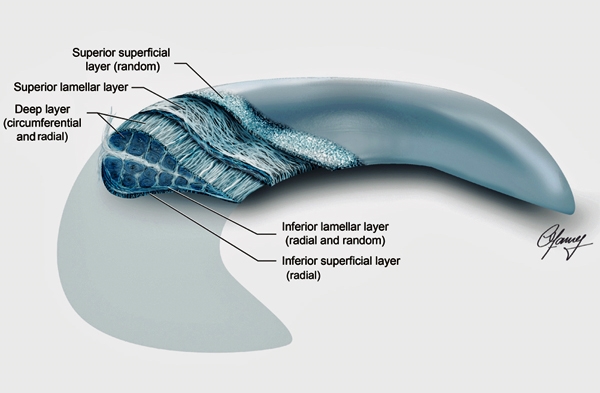
Figure 3. Collagen fiber arrangement in the meniscus. Collagen organisation should be considered as 3 layers: superficial, lamellar and deep. Collagen fibers are unstructured in the superior superficial layer but radially orientated in the inferior superficial layer. Amorphous collagen arrangement persists in the lamellar layer but is different from the superficial layer in that contains short, radially orientated fibers only at the posterior and anterior horns.