Motor
Examine muscles in order of innervation from proximal to distal
- Brachioradialis (BR)
- Extensor carpi radialis longus (ECRL)
- Extensor carpi ulnaris (ECU)
- Extensor pollicis longus (EPL)
- Extensor indicis proprius (EIP)
Interpretation:
- Complete weakness of wrist extension (ECRL and ECU)
- High radial nerve lesion
- Weakness of ulnar deviation in wrist extension (ECU) but good power of radial deviation in wrist extension (ECRL)
- Pathology distal to bifurcation of radial nerve
Radial tunnel syndrome
Injury between innervation of these muscles
- When testing finger extension, ensure the MCPJs also extend. IPJ extension alone is effected by the lumbricals (median/ ulnar nerves) so can give a false positive result
Sequence for radial nerve motor testing (proximal to distal)
Palpate the muscle/ tendon as you test each muscle group (not always shown to demonstrate anatomy)

Figure 10 Brachioradialis.With the elbow at 90° and the forearm in neutral pronation, flex the elbow against resistance and palpate the muscle

Figure 11 ECRL.Extend and radially deviate wrist against resistance

Figure 12 ECU.Extend and ulnarly deviate wrist against resistance
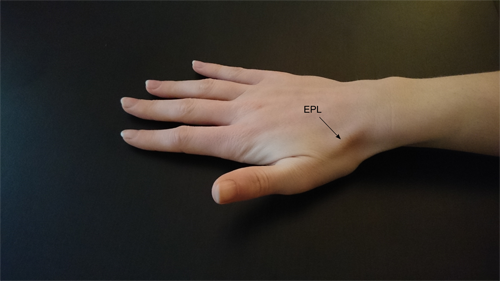
Figure 13 EPL.Thumb retropulsion

Figure 14 EIP .Point index finger with rest of fingers flexed to eliminate ED