Rheumatoid arthritis is a systemic disease, variably affecting many other systems as follows:
- Cardiac – pericarditis, cardiomyopathy, nodules causing conduction or valvular defects.
- Pulmonary – pulmonary fibrosis, pleural effusions, nodules (Figure 4) (granulomas), interstitial fibrosis, bronchiectasis
- Eye – scleritis (Figure 2), episcleritis, Sjogren's syndrome (autoimmune condition affecting exocrine glands) dry eyes and dry mouth. Decreased secretions from salivary and tear duct glands.
- Kidney – amyloid.
- Nervous system – entrapment peripheral neuropathies.
- Felty's syndrome (RA with splenomegaly and leukopenia) appears in patients with long-standing disease.
- Rheumatoid vasculitis.
- Still's disease (acute onset RA with fever, rash and splenomegaly).
- Lymphoid tissue proliferation.
Always ask about activities of daily living in the history especially relating to fine movements of the hand (doing buttons, holding a pen) as these joints are commonly affected[V1] .
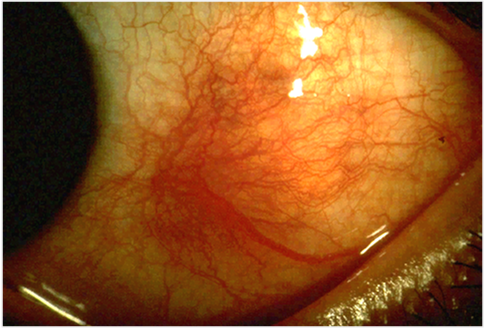
Figure 2. Scleritis
Figs 3. Pulmonary nodules.
Signs on examination
- Joint swelling (on palpation feels “boggy” due to synovitis), erythema, warm overlying skin, muscle wasting.
- Synovitis mainly affects wrists, MCP, and PIP joints in the hand.
Classic RA hand and wrist signs (Figure 4)
- Ulnar deviation of fingers
- Wrist subluxation
- Boutonniere deformity (PIP flexion, DIP extension)
- Swan-neck deformity (PIP extension, DIP flexion)
- Z-deformity of thumb
- Rupture of extensor tendons and muscle wasting

Figure 4. Rheumatoid wrist
Cervical spine
- Cervical spine involvement is important as it can cause atlanto-axial joint (Figure 6) and subaxial subluxation (Figure 7).
- Decreased space for spinal cord means that sudden movements of head or neck can cause cord damage and occasionally sudden death.
- X-rays must be taken prior to general anaesthesia in RA patients so anaesthetist can assess this prior to intubation.
- Other features on examination: rheumatoid nodules – swellings on elbows and fingers.
- Carpal tunnel syndrome – nerve compressed due to synovitis.

Figure 5. Cervical Myelopathy.Atlanto-axial subluxation in flexion.
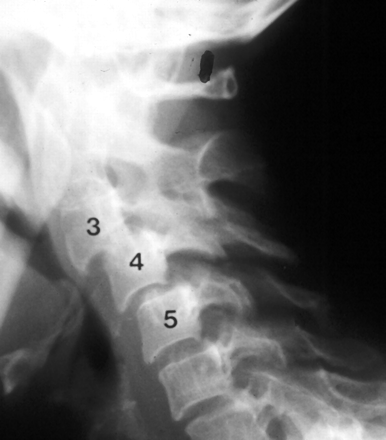
Figure 6. Rheumatoid Arthritis in the Cervical Spine. Subaxial subluxation C3-C5