The risk of contralateral slip varies from 18 to 60% which could justify prophylactic PIS of the contralateral hip even if it is asymptomatic. However, this is not free of risk and it should be weighed against the benefit.
In a review of 50 children with unilateral SUFE, (Stasikelis, Sullivan et al. 1996) tried to identify predictors for future contralateral slip. They found the modified Oxford bone age strongly correlated with the risk of development of a contralateral slip; contralateral slip developed in 85% of patients with a score of 16, in 11% of patients with a score of 21, and in no patient with a score of 22 or more. The modified Oxford bone age is based on appearance and subsequent fusion of the iliac apophysis, femoral capital physis, greater and lesser trochanter.
The posterior slip angle (PSA) was proposed by (Phillips, Phadnis et al. 2013) as a reliable predictor for contralateral slip. They examined 132 patients with SUFE and found the PSA was significantly higher in children who subsequently developed contralateral slip ( 17.2° ± 5.6°; N=42 vs. 10.8° ± 4.2°; N=90; P=0.001). If a posterior sloping angle of 14° were used as an indication for prophylactic fixation, 35 (of 42 = 83.3%) would have been prevented, and 19 ( of 90 = 21.1%) would have been pinned unnecessarily.
The followings may aid decision making (Alshryda, Jones et al. 2014):
- Age of the child (< 10 years is associated with a higher risk of bilaterality).
- Slips associated with renal osteodystrophy and endocrine disorders (a high incidence of bilaterality)
- Poor compliance of the child and family.
The nature of current slip (very bad slip occurred over a very short period of time may justify pinning the other side)
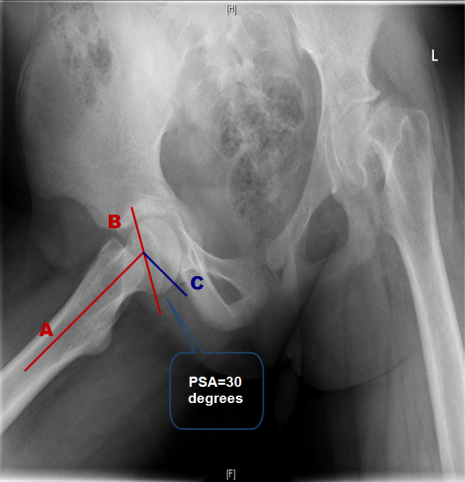
The posterior sloping angle (PSA) measured by a line (A) from the center of the femoral shaft through the center of the metaphysis,. A second line (B) is drawn from one edge of the physis to the other, which represents the angle of the physis. Where lines A and B intersect, a line (C) is drawn perpendicular to line A. The PSA is the angle formed by lines B and C posteriorly as illustrated.