The aim objectives of treatments are to reduce the hip, maintain the reduction while minimising complications. Achieving this depends on the child age, reducibility of the dislocation and available equipments. In general:
|
< 6 months
|
Pavlik Harness
|
|
6-18 months
|
Closed reductions + tenotomy+ hip spica
|
|
18-30 months
|
Open reduction ± Pelvic ±femur+ hip spica
|
|
> 30 months
|
As above or leave it dislocated.
|
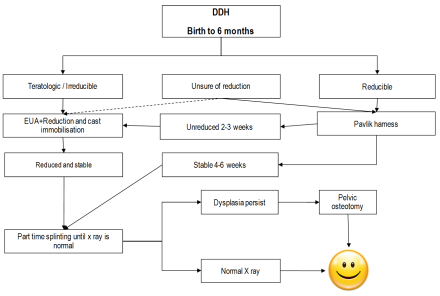
DDH flow chart management (Birth to 6 months). The figure is courtesy of Postgraduate Paediatric Orthopaedic book, Cambridge University Press©
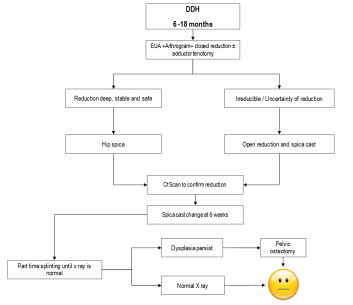
DDH flow chart management (6 – 18 months). The figure is courtesy of Postgraduate Paediatric Orthopaedic book, Cambridge University Press©
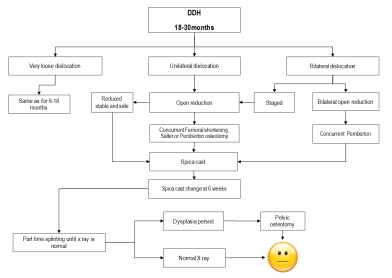
DDH flow chart management (18- 30 months). The figure is courtesy of Postgraduate Paediatric Orthopaedic book, Cambridge University Press©
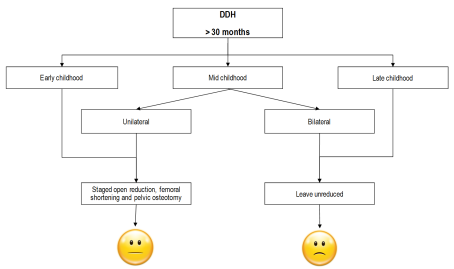
DDH flow chart management (over 30 months). The figure is courtesy of Postgraduate Paediatric Orthopaedic book, Cambridge University Press©
The upper age at which a successful reduction can be carried out has been debated. It is accepted that reduction is recommended for unilateral dislocations in children up to 10 years old and for bilateral dislocations in children up to 8 years. The natural outcome of untreated bilateral dislocations is likely to be better than the results of the reduction of both hips.
Several splints and braces are used to treat children less than 6 months with dislocated hips; the commonest by far is Pavlik harness. It is relatively easily to apply and most babies tolerate well. It allows motion within the range of stability. This motion is essential for stimulating the growth of acetabulum. The usual position to reduce the hip is 100 degrees of flexion and about 60 degrees of abduction (provided the hip is reduced in this position). Excessive flexion may cause femoral nerve palsy or inferior dislocation while less flexion may cause the hip to re-dislocate. The front leg strap control the amount of flexion while the posterior leg strap controls the abduction. Excessive abduction may cause AVN and less abduction may cause re-dislocation. It is essential to frequently check the child with PH for hip reduction, hip development, and complications. In dislocated hip, it should be applied full time, however, for dysplasia without hip dislocation, it can used on part time basis. Recognised complications include failure of reduction, AVN (2.4%), brachial plexus injury, knee dislocation and femoral nerve palsy (2.5%).

A child in a Pavlik Harness.
Video link (child with femoral nerve palsy following Pavlik harness treatment)
https://www.youtube.com/watch?v=v3xEgfa5SH8
Older children or those who failed Pavlik are treated with closed reduction. This is usually performed under general anaesthesia combined with arthrogram to assess the quality of reduction. The range of motion (often called the safe zone) in which the hip remains reduced and the points of dislocation are noted. Adductor tenotomy and / or psoas tenotomy may become necessary to improve the safe zone. The reduced hip is usually maintained in a hip spica (hip abduction of about 45º, flexion of more than 90º and neutral hip rotation).

A child in a hip spica after open reduction of a dislocated hip. Note the position of the left leg ( 30 flexion ,30 abduction and 30 IR position).
Open reduction is indicated when the reduction is not possible or when the reduction cannot be maintained. Open reduction may be performed from medial approaches (< 1 year) or from an anterior approach (older children). The disadvantages of the medial approach are a limited view of the hip, inability to perform a capsulorrhaphy and the risk of AVN.
Pelvic osteotomy may be required to improve stability of the reduction. The three commonly used are Salter’s Innominate osteotomy, Pemberton pelvic osteotomy or acetabuloplasty. These are explained in more detailed in a separate chapter.
Femoral osteotomy may be required especially in older children. This could include shortening, varus, derotation or a combination depending on the stability requirement.
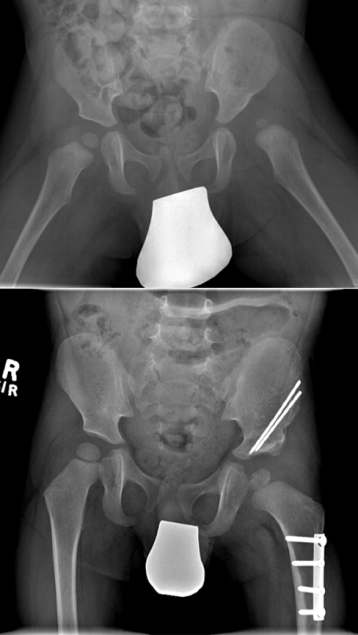
Plain radiograph of a child who underwent open reduction, femoral and pelvic (Salter) osteotomy.