Tibio-Femoral Angle (TFA)
- Angle formed by intersection of the two mid-diaphyseal lines of femur and tibia
Mechanical and Anatomical Axis Difference (MAD)
- Anatomical axis cross at the centre of knee
- Mechanical axis normally pass 8±7 mm medial to the centre of knee
Metaphyseal-Diaphyseal Angle (MDA)
- Angle formed by a line connecting the most distal point on the medial and lateral beaks of the proximal tibial metaphysis and a line perpendicular to the anatomic axis (or lateral cortex) of the tibia
- More than 10°
Epiphyseal-Metaphyseal angle (EMA)
- Angle formed by a line through the proximal tibial physis parallel to the base of the epiphyseal ossification centre with the most distal point on the medial beak of the proximal tibial metaphysis
- More than 20°
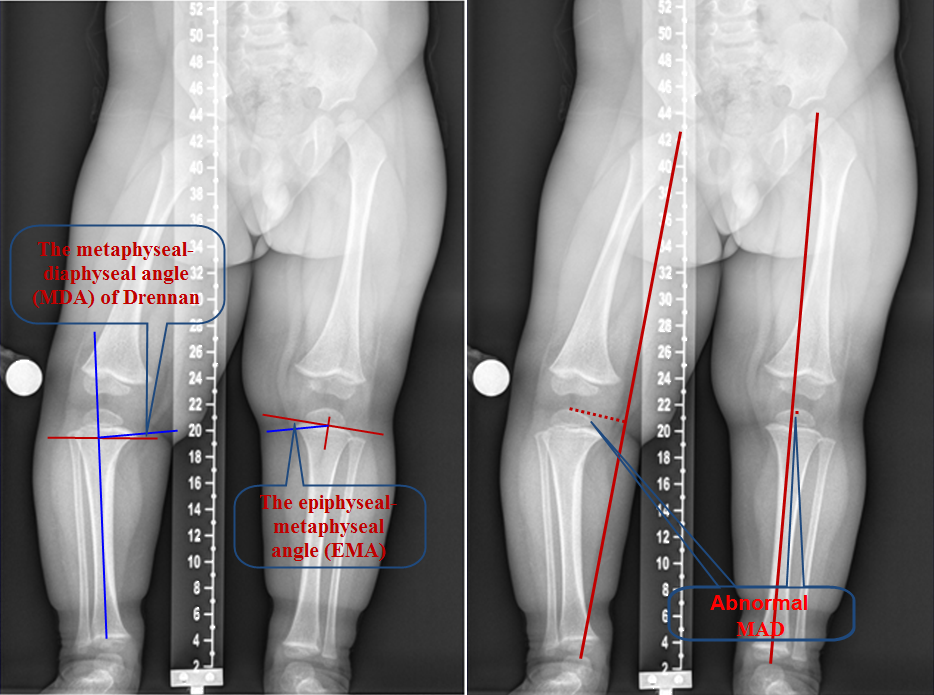
Common radiological measurements when assessing genu varum or valgum; TFA, MAD, MDA and EDA (see text for description).