- There are two distinct forms: proximal focal femoral deficiency (PFFD) and congenital short femur (CSF).
- PFFD describes a deformity in which there is discontinuity (with loss of various length of the femur) between the femoral neck and shaft.
- CCSF describes short but full femur with no bony loss or discontinuity. In most cases.
- The cause of the femoral deficiency is unknown; however, it can be part of genetically transmitted syndromes.
- Three classifications are in use:
- Aitken’s
- Gillespie and Torode
- Paley
Gillespie and Torode recognised 3 types:
Group A: Femur is short by about 20% but child can weight bear on the affected leg.
Group B: The femur is short by 40% (the foot of the affected level is at level between the knee and mid-tibia compared with the normal side).
Group C: The thigh is short and bulbous and the leg is externally rotated with the foot at or near the level of the other knee.
Paley’s classification:
Type I: Intact femur with mobile hip and knee:
a) Normal ossification proximal femur
b) Delayed ossification proximal femur
Type II: Mobile pseudarthrosis (hip not fully formed, a false joint) with mobile knee
a) Femoral head mobile in acetabulum
b) Femoral head absent or stiff in acetabulum
Type III: Diaphyseal deficiency of femur (femur does not reach the acetabulum)
a) Knee motion > 45 degrees
b) Knee motion < 45 degrees
Type I is further sub-classified into:
0) No factors to correct before lengthening
1) One factor to correct before lengthening
2) Two factors to correct before lengthening
3) Three factors to correct before lengthening
4) etc.
Examples of factors requiring correction prior to lengthening of femur are NSA < 90°, delayed ossification proximal femur, central edge angle (CEA) < 20°, subluxing patella and/or dislocating knee.
Treatment must be tailored to individual patients based on LLD, hip and knee stability, femoral rotation, proximal musculature, foot condition, availability of the expertise and patient and family motivation. The two broad options are reconstructive surgery or amputation and prosthetic replacement.
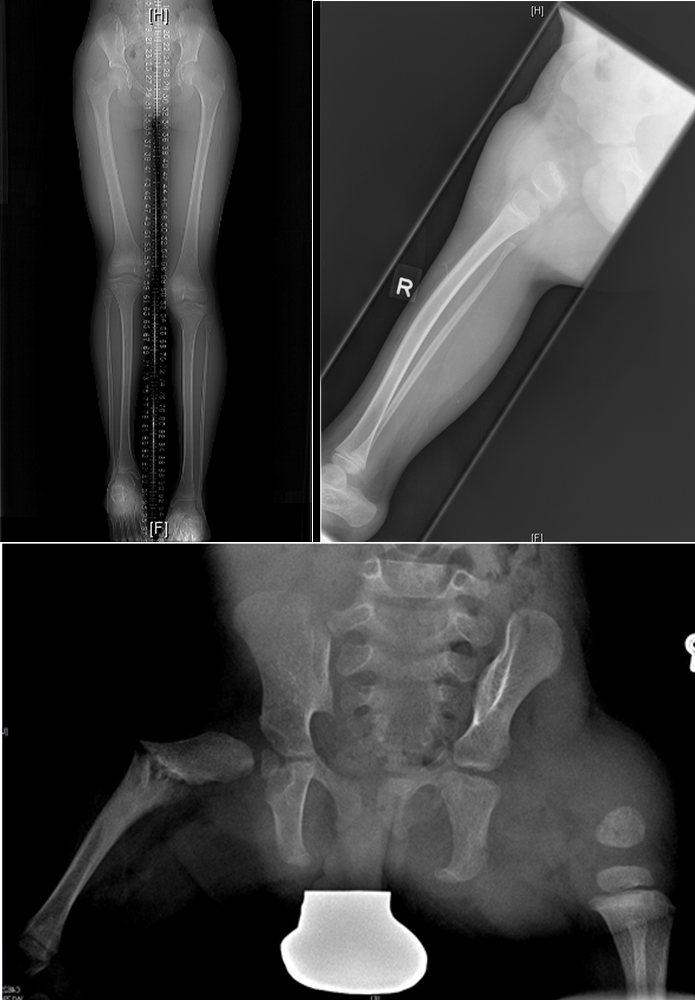
Plain radiographs showing various severity of CFD, type A (top left), Type C (top right) and type B and C in bottom image.