Pathogenesis
- There are several routes where bacteria invade joints
- Haematogenous spread
- Direct inoculation (surgery or trauma)
- From adjacent Osteomyelitis
- Bacteria release endotoxins and body respond by releasing cytokines, such as tumor necrosis factor and interleukin-1.
- These cytokines stimulate the release of proteolytic enzymes.
- This combination of factors leads to destruction of the synovium and articular cartilage.
Clinical Features
- Constitutional system (fever, malaise, anorexia, irritability and not feeding)
- Loss of function (Limp, inability to weight bear, pseudo-paralysis in the neonate.
- Joint effusion, overlying erythema, restricted range of motion.
Investigation
Blood test
- WCC
- ESR (doesn't start elevation until 48 hours)
- CRP may be a better marker in older children as it is elevated ithin 6 hours and peaks over the next 48 hours.
Imaging studies
- Non invasive and inexpensive
- Operator dependent
- Useful tool to detect joint effusion
- It can also assess the extra articular structures (joint capsule, periosteum, metaphyseal bone and adjacent soft tissues).
- Cannot differentiate between infection and non- infectious inflammatory arthropathy.
Figure 1.5.1
Ultrasound images of the right hip in a 3-year-old female. A large effusion is evident (white arrow) with layering suggestive of debris (curved red arrow). Capsular thickening (red arrow) is also evident. Image is courtesy of Postgraduate Paediatric Orthopaedic, Cambridge University Press.
Joint Aspiration
- Should be done under complete aseptic technique (first do no harm).
- Invasive
- Findings can be inconclusive
- Defining infection (may vary among various institutes)
- Positive culture, although can be negative in up to 40% cases of septic arthritis
- Synovial leukocyte count more than 50,000/mm3 and 75% polymorph presence indicates infection. Or more than 5 pus cell (WCC) per high power field
Differential Diagnosis
- Haemarthrosis
- Traumatic effusion
- Transient synovitis (see below)
- Reactive arthritis
- Lyme arthritis
- Juvenile rheumatoid arthritis ( risk of blindness, if you suspect refer to rheumatologist asap)
- Arthritis of acute rheumatic fever
- Osteomyelitis
- Tumours
- Perthe’s disease
Differentiate between Septic arthritis and Transient synovitis:
Transient synovitis is by far more common than septic arthritis; however the latter needs urgent attention. Kocher et al (1-3) in several studies proposed criteria (named Kocher’s criteria) to help differentiate between them.
He identified four independent predictors to differentiate between Transient synovitis and septic arthritis; Fever > 38.5°c, inability to weight bear, ESR >40, WBC >12,000/mm3.
Kocher’s Criteria
|
No. of positive predictors
|
(% risk of septic arthritis)
Kocher 1999
|
(% risk of septic arthritis)
Kocher 2004
|
|
0
|
0.2
|
2
|
|
1
|
3
|
9.5
|
|
2
|
40
|
35
|
|
3
|
93.1
|
72.8
|
|
4
|
99.6
|
93
|
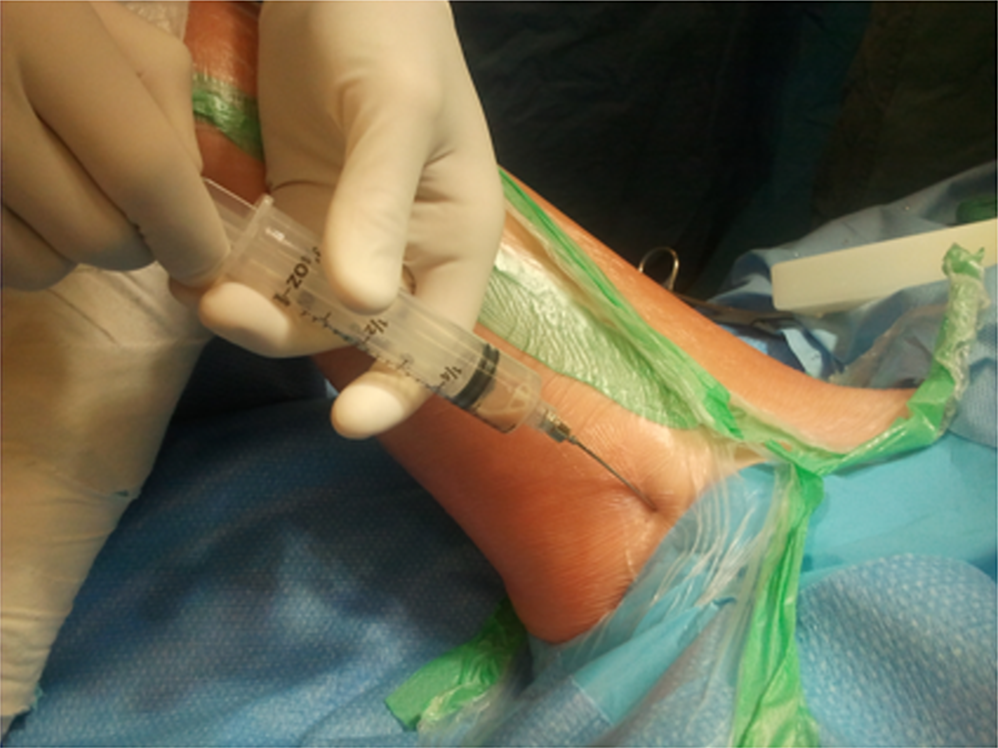
Figure 1.5.2. Medical approach to aspirate a hip Image is courtesy of Postgraduate Paediatric Orthopaedic, Cambridge University Press
Management
Principles of management of acute septic arthritis are:
- Adequate and prompt drainage of the joint
- Antibiotics to diminish systemic effects of sepsis
- Rest joint
- Antibiotics should be administered once the diagnosis is made. Sample should be sent for gram stain, culture and cell count.
- The choice of antibiotic therapy depends the local guidelines and adjusted according to the culture results.
- Ideally this should be in close liaison with microbiologist or an infection control specialist with an interest in MSK.
- Duration and route of administration is controversial and most units have their own local guidelines.
- The current trend is IV antibiotic until clinical and biochemical resolution then switch to oral antibiotics for 4-6 weeks of treatment.
- Controversy exists about open surgical drainage, arthroscopic drainage and multiple aspirations as good results with all three methods have been reported. The essence of success is an adequate drainage.
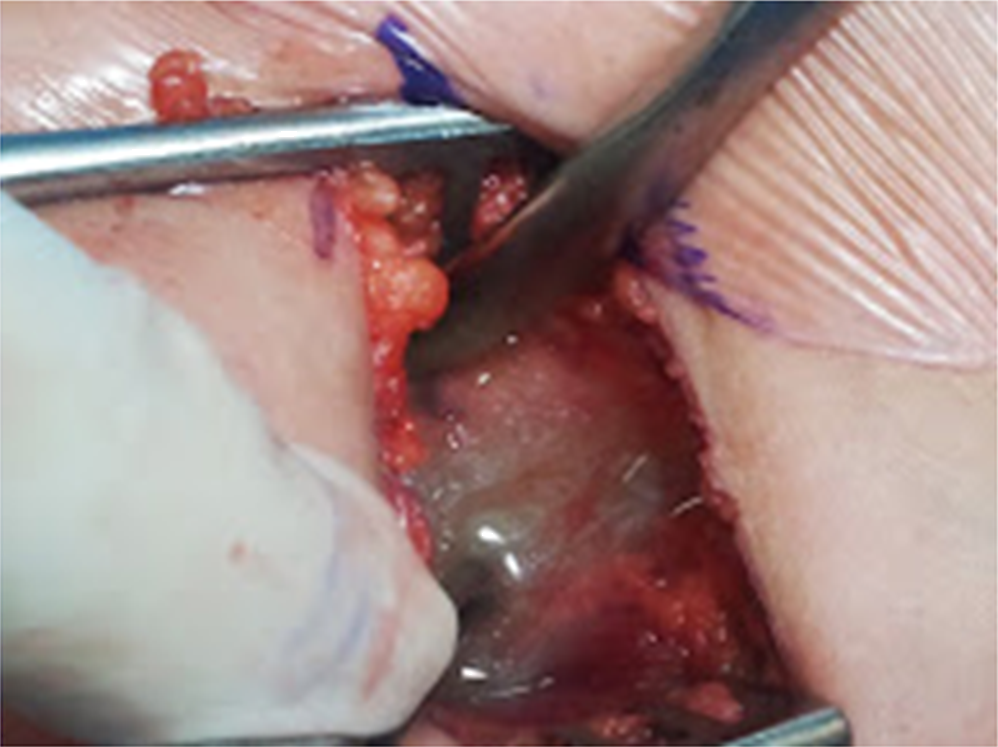
Figure 1.5.3. Hip joint is full of pus
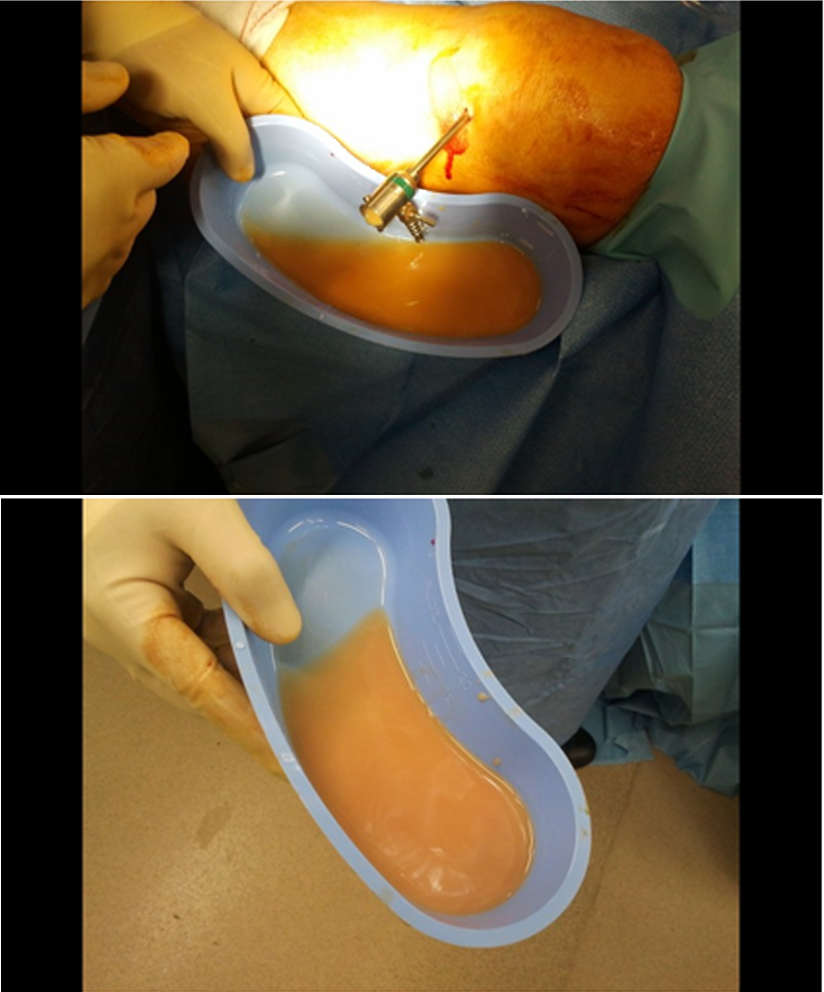
Figure 1.5.4 Arthroscopic washout of an infected knee