- The severity of cerebral palsy (CP) can vary from subclinical findings to very severe and disabling deformities.
- Symptoms and signs usually get worse as the child grows. Moreover, children develop compensatory or secondary deformity to improve their functional capability. This makes surgical decisions somehow unpredictable.
- The introduction of Botox treatment and gait analysis has changed the approach to treating children with CP from addressing single problems one at a time (commonly called the Birthday Syndrome) to a single event multilevel surgical approach (SEMLS) where multiple deformities are addressed simultaneously.
- There are obvious benefits of SEMLS in carefully selected patients (one anaesthetic, one admission, better outcomes, less cost) however, it can be less predictable and the risk of surgery is higher.
- Even in SEMLS, surgeons occasionally do not correct every deformity particularly if they are minor ones. Future “tidying operation” may become necessary to deal with uncorrected deformities if they impair function.
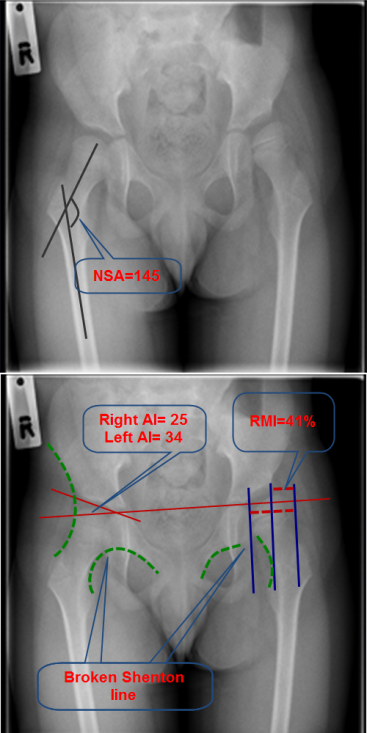
Plain pelvic x-ray of a child with CP showing commonly measured parameters. NSA is the angle between the femoral shaft and neck (125-135°). Reimer’s migration index (RMI) is the percentage of uncovered head (= width of the uncovered head / the width of the head X 100). Normal RMI is less than 30%. Traditionally, RMI between 30-50% is considered as an early subluxation, > 50% as a moderate subluxation and > 90% as a dislocation.
Orthopaedic procedures that are useful in CP can be divided into:
Soft tissue procedures:
- Tenotomy
- Tendon transfer
Both inevitably weaken the tendons on a permanent basis, therefore bony procedures are often preferred where possible.
Bony Surgery:
Bony surgery is required to realign the bones and restore optimum lever functions. The following bony surgery is commonly performed:
- Shortening (e.g. proximal femur)
- Lengthening (Calcaneum)
- Derotation (femur or tibia)
- Varus (femur)
- Extension (proximal or distal femur)
- Combined (femoral VDRO).
- Pelvic osteotomy (e.g. Dega osteotomy)
- Epiphysiodesis
- Arthrodesis
- Salvage surgery such as excision of the proximal femur