- Comprise 50% to 70% of all elbow fractures seen most frequently in children aged 3 and 10 years.
- The high incidence of residual deformity and the potential for neurovascular complications make these fractures a serious injury.
- Fall on an outstretched hand with elbow hyperextension is the main mechanism of injury, enabling the olecranon process to act as a fulcrum for injury.
- A posteriorly applied force with the elbow in flexion creates a flexion-type SCH (2-5% cases) (figure 6.5.1).
- Several radiographic features have been proposed to confirm a subtle supracondylar fractures, differentiate SCH # and condylar fractures and predict the operative difficulty that surgeons may encounter while stabilizing these fractures (figure 6.5.2).
- Wilkins modification of the Gartland Classification for supracondylar fractures (Figure 6.5.4).
- Undisplaced (Type I). In the absence of a clear bony injury, a posterior fat pad sign is an important sign of an occult intra-articular or supracondylar fracture. Very young children may have severe injuries with very little bony abnormality due to the lack of ossification
- Angulated (Type II)with intact posterior cortex (IIA= angulation only, IIB= with rotation)
- Complete displacement (Type III) (IIIA= posteromedial, IIIB=posterolateral)
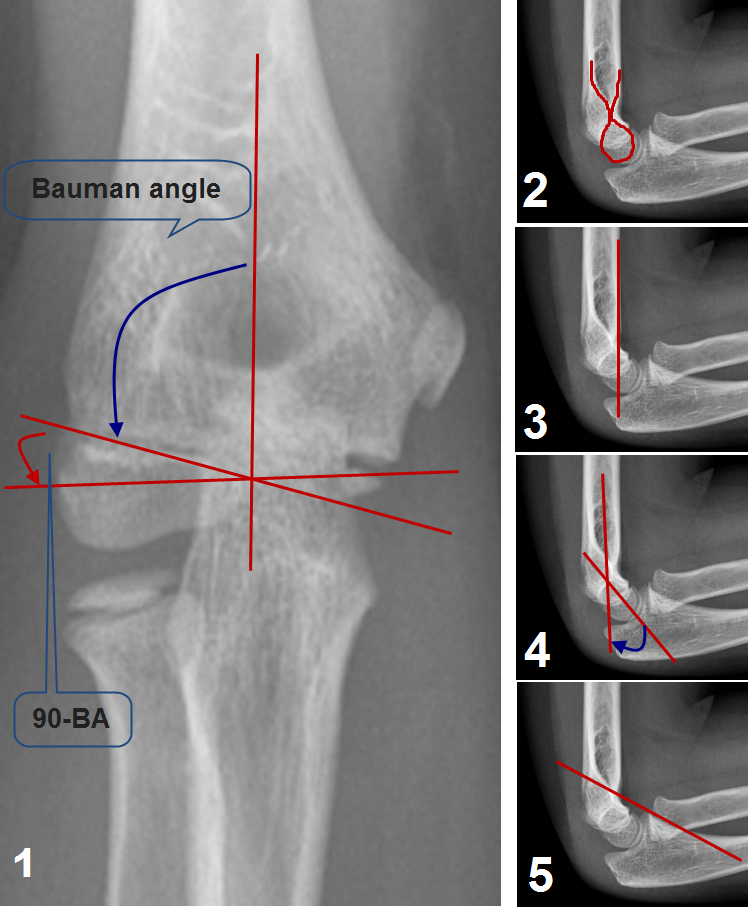
Radiological features of the paediatric elbow: image 1-Bauman’s angle formed by the capital physeal line and the long axis of the humerus (normally is 75-80°). The carrying angle, it is the natural valgus of the elbow joint. It can be measured by subtracting the Bauman’s angle from 90°. Image 2-The teardrop or the hour glass, the narrow part represent the coronoid fossa. The inferior portion of the teardrop is the ossification center of the capitellum. On a true lateral projection, this teardrop should be well defined (useful sign of true lateral projection).Image 3- The anterior humeral line drawn along the anterior border of the distal humeral shaft, it should pass through the middle third of the ossification center of the capitellum. Image 4- shaft-condylar angle which is the angle between the long axis of the humerus and the long axis of the lateral condyle (normally 40°). Image 5- Coronoid Line directed proximally along the anterior border of the coronoid process should barely touch the anterior portion of the lateral condyle. Images are courtesy of Postgraduate paediatric orthopaedic, Cambridge University Press.