- There is fixed lateral dislocation of a hypoplastic patella, lack of active knee extension and absence of the patella from intertrochlear fossa.
- Congenital patellar dislocation can be associated with Larsen’s syndrome, arthrogryposis, myelomeningocele, Down syndrome, nail-patella syndrome, Beckwith-Wiedemann syndrome, diastrophic dysplasia and PFFD.
- Ultrasound can be used to locate the patella and confirm the diagnosis.
- MRI can be used as part of preoperative assessment and planning.
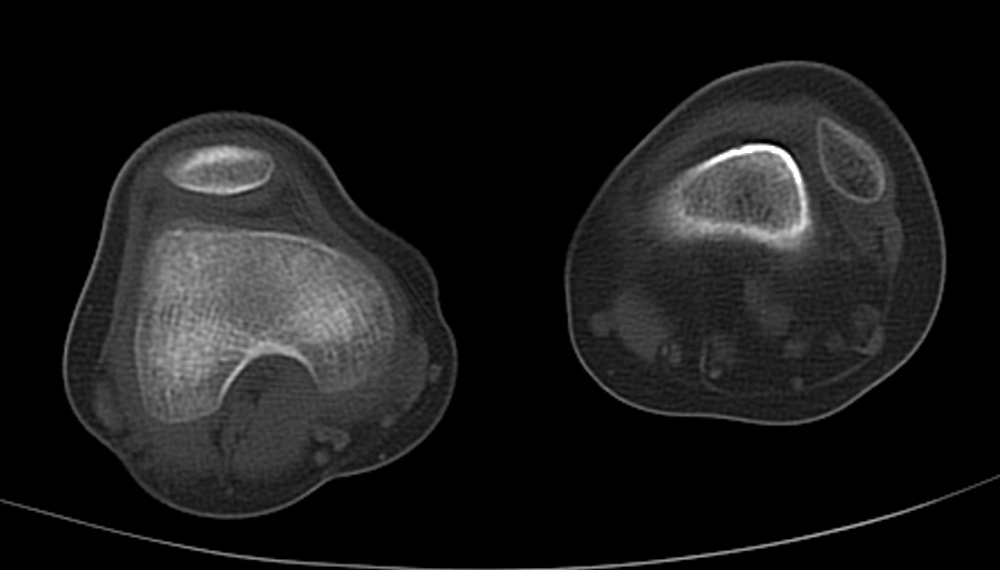
CT scan showing a hypoplastic patella dislocated laterally.

MRI scan showing a hypoplastic patella dislocated laterally and external torsion of the tibia in relation to the femur.