Abnormal spontaneous activity(Figure 6):
- Fibrillations
o Following an acute nerve transection, nerve fibres degenerate from the site of the lesion distally. Muscle fibres remain viable, but after about a week become hypersensitive due to the accumulation of acethylcholine. As a result they discharge spontaneously. The EMG needle detects this spontaneous discharge as single fibre discharge or fibrillation.
o Seen in neurogenic disorders, inflammatory conditions and muscular dystrophy.
- Fasciculations
o Are larger and more complex than a fibrillation.
o May be visible clinically.
o Occur in motor neurone disease, radiculopathy, neuropathy and thyroid disease.
o May be benign. Benign fasciculations are not associated with denervation changes but pathologic fasciculations usually are.
- Myotonia
o Discharge is provoked by gently stimulating the muscle.
o There is a varying frequency and amplitude that produces a characteristic noise described as the “dive-bomber” sound.
- Neuromyotonia
- Myokinia
The pattern of motor unit recruitment is affected by the force of muscle contractility. This has to be considered by the electromyographer when assessing motor unit recruitment.
- Reduced recruitment
May be caused by reduced contraction due to pain inhibition or lack of patient compliance, an upper motor neurone lesion, motor conduction block or partial denervation.
- Early recruitment
In primary muscle disease the recruitment pattern is described as early. Even at low force contraction, a full recruitment pattern is seen.
- Motor unit potentials
The amplitude, duration and number of phases may be measured to assess muscle denervation and the presence of re-innervation following nerve injury.
- Tremor
EMG is used in conjunction with NCS to make diagnoses of peripheral nerve lesions, neuromuscular junction disorders, motor neurone disease and primary muscle disease. Its strength lies in its ability to identify which particular muscle or muscle groups are pathological and then deduce from the spontaneous activity and motor recruitment pattern, the likely causes for the noticed abnormality.
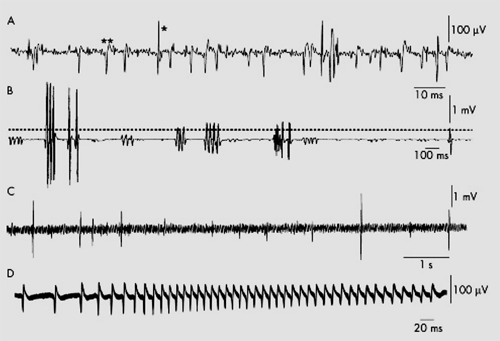
Figure 6 Abnormal spontaneous activity. (A) Fibrillations (*) and positive sharp waves (**) in an acutely denervated hand muscle. (B) Single, doublet, triplet, and multiple motor unit neuromyotonic discharges. Bursts of discharge are irregular in frequency and the intra-burst frequency of discharge is up to 200 Hz. (C) Fasciculations in the tongue in a patient with5 amyotrophic lateral sclerosis. The single discharges are irregular and occur on a background of ongoing EMG activity caused by poor relaxation. (D) Myotonic discharges in a patient with dystrophia myotonica. There is a characteristic waxing and waning in frequency.