- The United States Food and Drug Administration defines a skin disinfectant as a “fast acting, broad-spectrum and persistent antiseptic-containing preparation that significantly reduces the number of microorganisms on intact skin.”
- Before a patient’s skin is prepared for a surgical procedure, it should be cleansed of gross contamination (e.g. dirt, soil or any other debris). The antiseptics used to prepare the skin should be applied with sterile supplies and gloves or by a no-touch technique, moving from the incision area to the periphery. Use pressure, because friction increases the antibacterial effect of an antiseptic.
Alcohol
- The exact mechanism by which alcohols destroy microorganisms is not fully understood. The most plausible explanation for their antimicrobial action is that they coagulate (denature) proteins, such as enzymatic proteins, thus impairing specific cellular functions. Alcohols are generally effective against bacteria but do not, however, destroy bacterial spores (e.g. Clostridium difficile). It is also effective against fungi and most viruses with a lipid envelope (influenza, herpes simplex, adenovirus).19
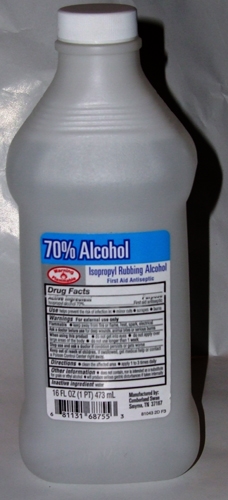
Figure 7. Alcohol skin prep
Chlorhexidine
- Most commonly formulated as a 4% aqueous solution in a detergent base; however, alcoholic preparations have been shown in numerous studies to have better antimicrobial activity than detergent-based formulations. Bactericidal concentrations destroy the bacterial cell membrane, causing cellular constituents to leak out of the cell and the cell contents to coagulate.
- It has a persistent antimicrobial action that prevents regrowth of microorganisms for up to 6 hours.
- It has little activity against bacterial and fungal spores. Fungicidal action varies with the species. It is active against lipophilic viruses (HIV, influenza, herpes).
- Blood and other organic materials do not affect the antimicrobial activity of chlorhexidine significantly, in contrast to their effects on povidone–iodine.19
- Povidone–iodine: iodophors are chemical complexes of iodine bound to a carrier such as polyvinylpyrrolidone (povidone) or ethoxylated nonionic detergents (poloxamers), which gradually release small amounts of free microbicidal iodine. The most commonly used iodophor is povidone–iodine. Preparations generally contain 1–10% povidone–iodine.
- The exact mechanism by which iodine destroys microorganisms is not known. It may react with the microorganisms’ amino acids and fatty acids, destroying cell structures and enzymes.
- It is bactericidal, mycobactericidal, fungicidal and virucidal but not sporicidal. Prolonged contact is required to inactivate certain fungi and bacterial spores.19

Figure 8. Chlorhexidine skin prep

Figure 9. Povidone–iodine skin prep
Triclosan and chloroxylenol
- 1% Triclosan has good activity against Gram-positive bacteria, but is less active against Gram-negative organisms, mycobacteria and fungi.
- It is active against enveloped virsuses, but less so against non-enveloped viruses.
- It has a sustained residual effect against resident and transient microbial flora, which is minimally affected by organic matter. However, it is less effective than 2–4% chlorhexidine gluconate when used as surgical scrub solutions.19

Figure 10. Triclosan skin prep
Octenidine
- Octenidine dihydrochloride is a novel bispyridine compound and an effective, safe antiseptic agent. The 0.1% compared favourably with other antiseptics with respect to antimicrobial activity and toxicological properties. It rapidly killed both Gram-positive and Gram-negative bacteria as well as fungi in vitro and in vivo. Octenidine is virucidal against HIV, hepatitis B virus and herpes simplex virus. Like chlorhexidine, it has a marked residual effect.19

Figure 11 Octenidine skin prep