Perthes disease
- Idiopathic AVN of proximal femoral epiphysis.
- See “paediatrics.”
Kohler’s disease (Figures 6 and 7)
- Avascular necrosis of navicular bone.
- Unclear aetiology.
- Usually children 4–7 years old.
- Boys > girls.
- Can be bilateral in 25%.
- The blood supply of the central one third of the navicular is a watershed zone which accounts for the susceptibility to AVN (and stress fractures).
- The navicular is the last bone to ossify, which also increases its vulnerability to mechanical compression and injury.
- Typically a self-limiting condition for 1–3 years after diagnosis.
- Radiographs show characteristic clerosis, fragmentation, and flattening of the navicular.
- Most tarsal navicular bones reorganise after the disease has run its course; some continue to be deformed but remain largely asymptomatic.
- Treated with rest, anti-inflammatories and occasionally a walking cast.

Figure 6. Weight bearing radiographs Kochler's disease
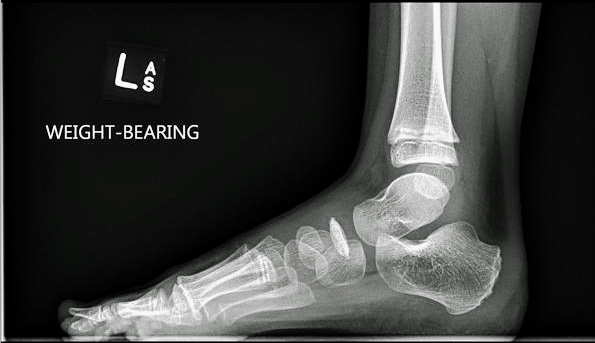
Figure 7. Lateral radiograph Kochler's disease
- Freiberg’s disease (Figure 8)
- AVN of second metatarsal head.
- Commonly in adolescents.
- Girls > boys.
- More common with a long second MT.
- Presents with localised pain, swelling and restricted movement.
- Radiogrpahs show a progression of sclerosis to flattening of the MT head to collapse and joint destruction in later disease.
Smillie classification – grades 1–5:
1. Magnetic resonance imaging diagnosed subchondral fracture
2. Dorsal collapse on X-ray
3. Collapse of dorsal MT head
4. Collapse of entire head with joint space narrowing
5. Secondary osteoarthritis
· Initial conservative Mx as above.
· Surgery may involve a dorsiflexion closing and shortening osteotomy or partial MT head resection.

Figure 8. Radiograph Frelberg's disease