- Humidity is the amount of water present in the vapour phase and is measured in hygrometers.9
- Absolute humidity is the mass of water present in a volume of gas and is expressed in mg/l:
HA = mass H2O (g)/volume of air (l).
- Relative humidity is the ratio of water partial pressure to saturated vapour pressure at a given temperature, and usually quoted as a percentage:
HR (%) = 100 x PH2O/SVP H2O
- The recommended humidity range in an operating room is 20–60% based on addendum d to ANSI/ASHRAE/ASHE standard 170-2008. Each facility should determine acceptable ranges for humidity in accordance with regulatory and accrediting agencies and local regulations.10
- Elevated levels of humidity are uncomfortable and can be associated with increased risk of infection.11,12
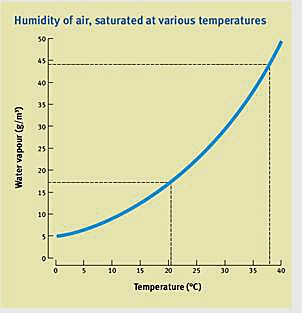
Figure 6. Theatre humidity